May 2022
Three Categories of Nerves

Peripheral neuropathy is a nerve disorder that can affect the feet. It typically causes the inability to feel sensations in the feet, and is prevalent among diabetic patients. Elevated glucose levels can cause neuropathy in the feet, and can be dangerous among diabetics. Neuropathy can affect many types of nerves. The most common are motor, sensory, and autonomic nerves. Motor nerves include those that allow us to walk, talk, and grasp objects. The pain that is felt from a cut is classified as a sensory nerve, and breathing, digestion, and heart functions are in the autonomic nerve category. Muscle weakness is associated with neuropathy, and can be caused by physical injury, arthritis, and diabetes. If you have a lack of feeling in your feet, it is strongly suggested that you are under the care of a podiatrist who can treat and help you to manage neuropathy.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Dr. John C. Lawlor from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact one of our our offices located in Cape Coral and LaBelle, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
When Heel Pain Is Caused by Plantar Fasciitis
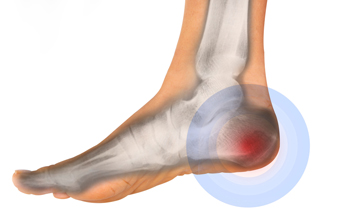
If you are experiencing pain on the bottom of your heel, there is a good chance that you may have a condition known as plantar fasciitis. Plantar fasciitis is an irritation and inflammation of the plantar fascia, which is a connective tissue that links the heel with the toes. Because the plantar fascia is located on the sole of the feet, it helps absorb the body’s weight, and can become overly stressed during walking, running, and jumping movements. Plantar fasciitis is the most common cause of heel pain and can make it difficult to walk. Common risk factors for plantar fasciitis include making certain repetitive movements (as in running) obesity, sudden weight gain (as in pregnancy), or by having flat feet or high arches or a tightened Achilles tendon. If you believe you have plantar fasciitis, make an appointment with a podiatrist to be properly diagnosed and to receive prompt and proper treatment.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. John C. Lawlor from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact one of our our offices located in Cape Coral and LaBelle, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Warts Have Wart Seeds

Plantar warts appear on the bottom of the foot. They grow inward as a result of the constant pressure that is exerted on the feet from standing and walking. They are caused by HPV, human papillomavirus, and can enter the body through small cuts in the feet. It is suggested to wear appropriate shoes while in public swimming areas and locker rooms, as this may prevent the spread of the virus. A plantar wart looks like a small area of hardened skin, and it generally has tiny black dots in the center. These are small, clotted blood vessels that are referred to as wart seeds. This type of wart generally causes severe pain and discomfort, and it may be difficult to walk. Patients who have a compromised immune system, in addition to people who are diabetic, may be prone to getting plantar warts. It is suggested that if you have a plantar wart to speak with a podiatrist who can guide you toward the best treatment methods.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. John C. Lawlor from Florida. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact one of our our offices located in Cape Coral and LaBelle, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Are Bunions Affecting Your Everyday Life?
Do I Have Toenail Fungus?

Toenail fungus, or onychomycosis, is an infection of the toenail that causes the nail to become discolored, thick, and prone to cracking and breaking. There is typically no pain associated with toenail fungus unless it becomes severe. Fungal nail infections are caused by different types of yeasts or molds in the environment that can get into the nail and cause an infection. The elderly, diabetics, those with weakened immune systems or blood circulatory problems, and those with athlete’s foot are more apt to get toenail fungus. To prevent toenail fungus, regularly wash and dry the feet, clip toenails straight across, do not walk barefoot in public areas, and beware of those who might have athlete’s foot as it is highly contagious. Visit a podiatrist to have your toenails checked if you suspect you have toenail fungus for a diagnosis and suggestions for treatment.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Dr. John C. Lawlor of Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact one of our our offices located in Cape Coral and LaBelle, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
When Cracked Heels Need Professional Care

While cracked heels may be considered by most to be an unsightly and mildly uncomfortable nuisance, they can develop into a more troublesome and serious condition in certain cases. Cracked heels can often improve with home treatment—such as by sloughing off dead skin in the shower with a pumice stone or by applying foot cream at night and covering the feet with cotton socks. However, the elderly, and people with certain medical issues should not attempt to treat cracked heels at home. Cracked heels that are allowed to deepen may bleed, and become painful or even infected. Severely cracked heels can be particularly problematic in older adults, or people with diabetes, eczema, psoriasis, or thyroid issues, and should be attended to by a podiatrist to help treat them properly and safely, and to avoid the possible development of cellulitis or a foot ulcer.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Dr. John C. Lawlor from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact one of our our offices located in Cape Coral and LaBelle, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.









